What is Dry Needling and How Does It Work With Physical Therapy?
Back to physical health resource hub
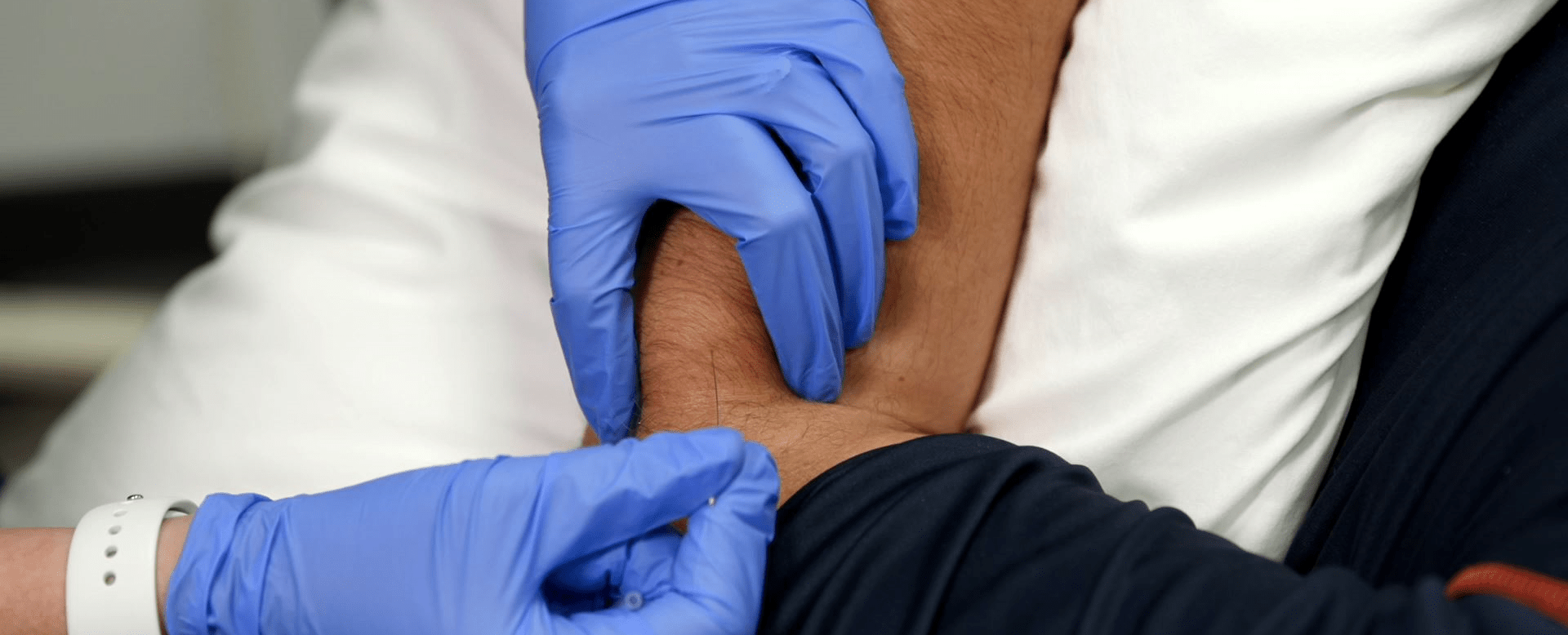
Though the term “Dry Needling” may sound a little ominous, it is a very effective form of therapy that is growing in popularity and usage. It involves the use of needles to stimulate and break up knotted or hard muscle tissue – called “trigger points” – usually located deeper in the body.
It’s called “dry” because the needle isn’t injecting a fluid – unlike, say, a needle used to inject a vaccine. The sole purpose of these dry needles is to treat the trigger points.
According to Jennifer Bruck, PT, DPT, CMTPT, physical therapist at Brooks Rehabilitation, trigger points can be “active” or “latent.” Active means that the trigger point is actively causing pain, while latent is not causing pain currently, but can be set off to generate pain. In addition to pain, trigger points can affect the motor patterns so that muscle firings or mechanics are not normal. Trigger points can be superficial or deeper.
Dry needling side effects in general are just like any other needle stick: There’s the standard risk of bleeding, bruising, or infection. “The most typical side effect is going to be soreness,” said Dr. Bruck. “You’re going to feel like you had a really good muscle workout – like going hard at the gym. Because essentially what I’m doing is fatiguing out that muscle to make it relax.”
How Dry Needling Works with Physical Therapy
Dr. Bruck uses this therapy on her patients and is also helping to train other Brooks therapists. “In a typical dry needling session, we palpate and localize a trigger point, which is some sort of muscle dysfunction. Typically what we do is find a tightened muscle tissue area, known as a taught band. Usually in the middle of that is the trigger point. We use the needle to help disrupt the muscle internally. I’m essentially going in and breaking it up so that it calms down.”
For these deeper, intramuscular trigger points, dry needling can be quicker and more effective than traditional physical therapy treatments. “With a lot of patients, you don’t need to do dry needling every single visit that they come in,” said Dr. Bruck. “You can help clean up some of that trigger point and problem in five or six visits, and then they don’t need it anymore. This is especially true if it’s very localized. If you have a muscle that has that one spot that’s just super, super hot on a patient, it can help calm it down a lot, and more quickly than manual therapy.”
Dry Needling Precautions
Dr. Bruck explains that patient selection is also key. “You need to make sure that the patient doesn’t have any potential contra-indications or precautions,” said Dr. Bruck. “So, if somebody has some sort of bleeding disorder or is on blood thinners, you want to be cautious, as using a needle may lead to increased risk of bleeding. Similarly, you may not offer it to someone who is more prone to infections, because anytime you pierce the skin with a needle, there’s the possibility. Last, but not least, are patients with a needle phobia. If you’re very much scared of needles, the last thing you probably want is dry needling.
“So, patient selection has a lot to do with our training. First, being manual, therapy-based clinicians to begin with as a physical therapist, and second, the extensive dry needling training. You draw on that training and use your clinical reasoning skills to identify what patients would be appropriate.”
Dry Needling Vs. Acupuncture
An obvious question about dry needling is its comparison to acupuncture. While both disciplines use the same type of filiform needle (solid, sterile and single use), the similarities end there. “It’s incredibly different from acupuncture,” said Dr. Bruck. “With dry needling, based on Western medicine, you’re going into a specific part in the muscle that’s dysfunctional. Whereas with acupuncture, based on Eastern medicine, there’s different points and meridians throughout your body that you’re trying to use the needle superficially, not intramuscularly, more skin level, to help assist with the flow of energy, or ‘chi.’”
Type of Training Therapists Need for Dry Needling
Currently, the American Physical Therapy Association (APTA) does not regulate training for dry needling; training and continued competency are handled by each state, e.g., the Florida Board of Physical Therapy. Dr. Bruck’s credential is “CMTPT” – certified myofascial trigger-point therapist, “Myofascial” is the dense tissue which surrounds, covers and separates all muscles and bones. CMTPTs are thoroughly trained in dry needling and acquire a very extensive knowledge of anatomy and physiology.
Find a Brooks Location Near You
Interested in receiving dry needling services? Reach out to one of our outpatient clinics that provides dry needling and book an appointment today.


