Treatment for Long COVID Symptoms Includes Rehabilitation Therapies

Back to physical health resource hub
Physical therapy, along with other rehabilitation therapies, have begun to play a critical role in managing some of the symptoms people are experiencing from long COVID.
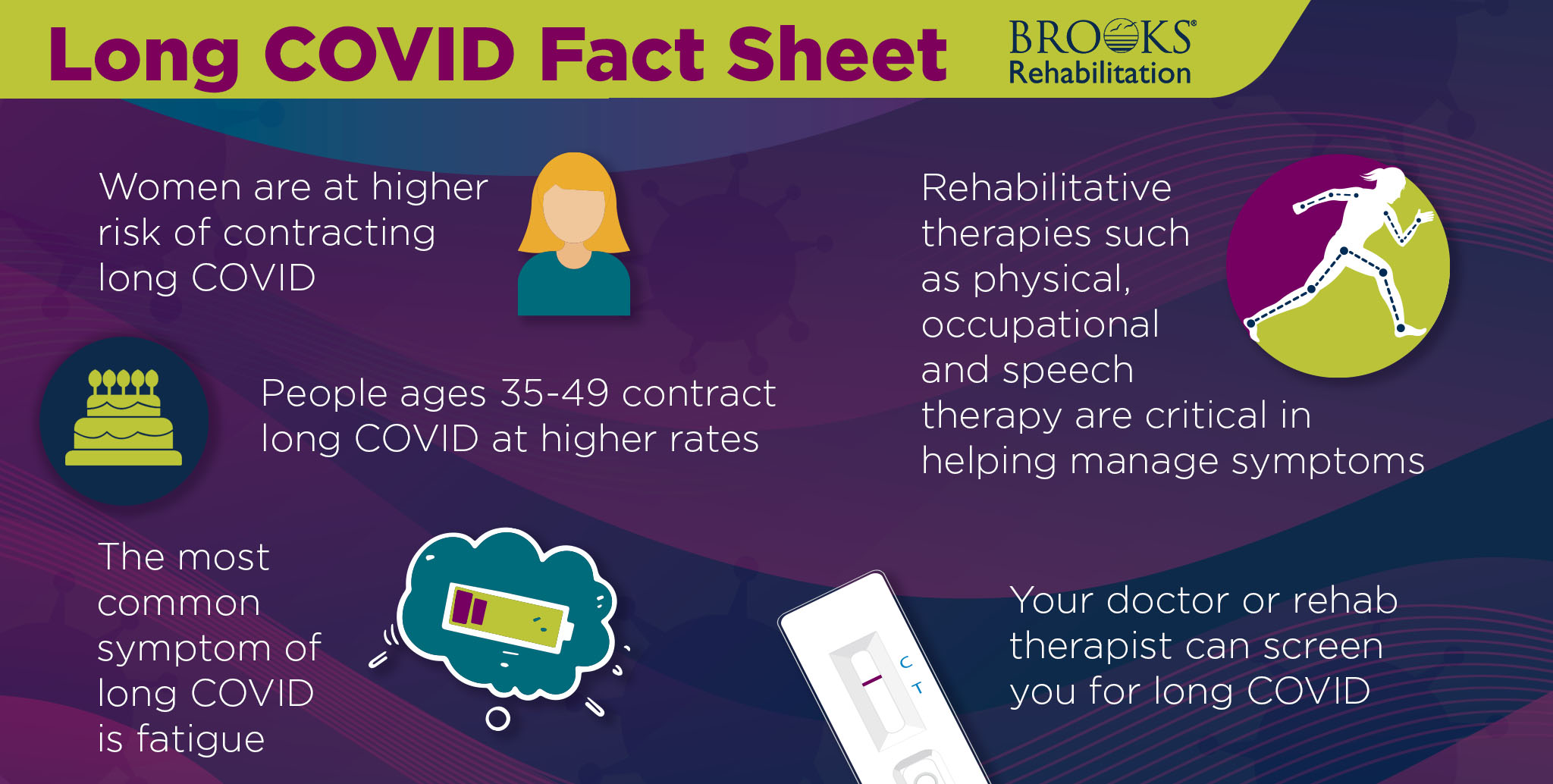
According to Centers for Disease Control and Prevention, about 6.9% of people develop long COVID after an acute COVID infection.
Long COVID symptoms include balance issues, fatigue, muscle aches and joint pain, brain fog and heart problems. For some people, the symptoms will go away after three months, for others it can continue for years.
There is no cure for long COVID. However, people suffering from the condition can manage their symptoms through medications and rehabilitative therapies such as physical therapy, occupational therapy and speech therapy to improve their quality of life.
Research is still being conducted to better understand this condition and develop more comprehensive treatments.
This article will cover the following topics:
- Symptoms of long COVID
- How rehabilitation therapies help manage symptoms
- Who can diagnose long COVID
- Who is at risk
- What to expect from therapy treatment
- Treatment plan for long COVID
- Where rehabilitative treatments take place
Symptoms of Long COVID
Long COVID affects each person differently. Some symptoms may also mimic other conditions, such as chronic fatigue syndrome making it difficult to identify.
“In some cases, an individual’s physical experience was so taxing that they didn’t recognize cognitive symptoms until it became an issue,” said Stephanie Richardson, MS, CCC-SLP, speech therapist at Brooks Rehabilitation.
According to the National Institute of Health, possible symptoms include the following:
Fatigue: Fatigue is one of the primary symptoms of long COVID. Tiredness or fatigue often interferes with everyday activities. It may become worse after physical or mental activity.
Balance issues: Although researchers need more studies completed, balance issues may occur due to changes in the vestibular system. The vestibular system is in the inner ear and plays a role in balance. Some studies indicate that a COVID infection can lead to inner ear infections, which disrupt the vestibular system and balance.
Brain fog: Brain fog involves problems thinking, remembering and concentrating.
“Brain fog can become an ongoing problem for some people with long COVID,” said Richardson. “It is impacting their memory, attention and problem solving. It can affect daily life and returning to daily routine activities such as cleaning, cooking, managing daily household duties and even prevent someone from returning to work.”
Muscle aches and joint pain: Muscle aches and joint pain can lead to reduced mobility, increased deconditioning and lost time from work.
Heart problems: Heart problems can vary in severity but may include irregular heart rhythms, chest pain and fainting. Heart issues can lead to problems with exercise tolerance, breathing and fatigue.
Respiratory difficulties: Lasting breathing issues can develop with long COVID. Some of these symptoms may include shortness of breath and a chronic cough. Respiratory symptoms can lead to poor exercise tolerance, decreased mobility and worsening deconditioning.
Emotional issues: Mood change and mental health difficulties, such as anxiety and depression, can also develop. Physical symptoms and decreased functioning further contribute to emotional problems.
How Rehabilitation Therapy Helps Manage Long COVID Symptoms
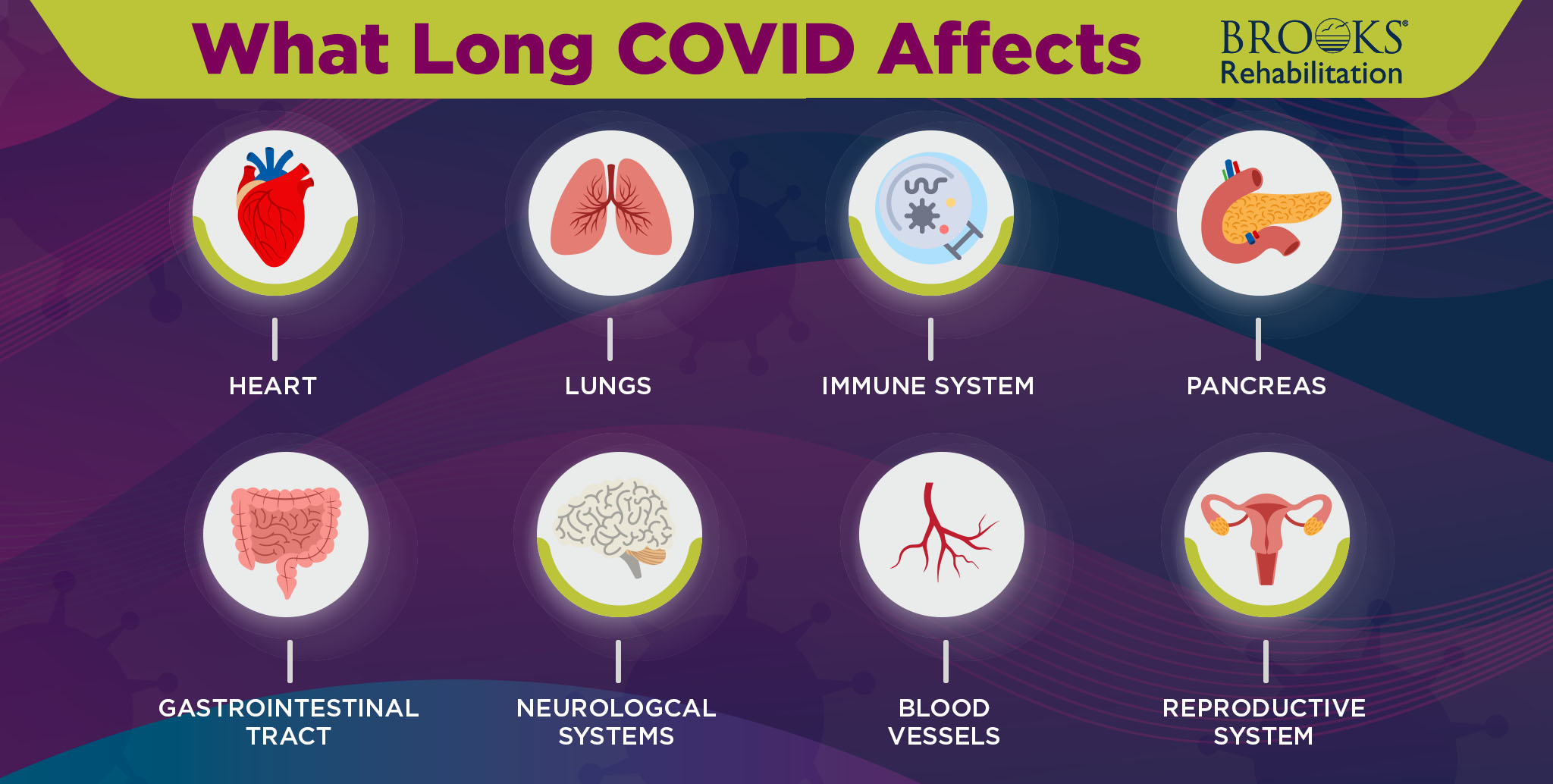
Long COVID can affect a wide range of organs and systems, which requires a combination of therapies and treatments.
“A multi-discipline approach focuses on the full picture,” said Richardson. “Physical therapists and occupational therapists can help improve physical symptoms. As physical symptoms improve, it can help boost confidence and promote improvement with cognitive problems, speech and other issues.”
The different types of therapies that fit into a treatment plan for long COVID, include:
Physical therapy
Patients with long COVID may have trouble breathing and be experiencing fatigue. Symptoms can make even simple tasks, such as climbing stairs, challenging. This then causes low endurance and poor muscle strength. Physical therapy can help increase endurance and muscle strength.
“Physical therapy can help with balance issues, weakness and deconditioning,” said Dellwo. “We work with patients to improve their strength and endurance, as well as improve balance and reduce fall risk.”
Therapy sessions vary in their approach. Sessions may include different types of exercises that improve range of motion, strength, balance and aerobic functioning.
Improving physical symptoms, such as fatigue, may also improve emotional symptoms, including depression and anxiety.
Occupational therapy
Occupational therapy is also helpful to help treat long COVID symptoms. OTs help patients build activity tolerance that improves doing activities of daily living, such as cooking, personal care and household chores.
Therapists may help patients develop new ways of doing activities. They may also introduce using adaptive equipment such as a reacher to make tasks easier.
Making everyday activities easier helps conserve energy and eases fatigue. OTs may also develop strategies to improve sleep hygiene, helping reduce fatigue.
Speech therapy
Speech therapy may also treat symptoms related to long COVID. “We see people with brain fog, which can lead to communication problems,” said Richardson. “We also see people with vocal dysfunction and swallowing impairments caused by respiratory issues or gastrointestinal sensitivities.”
Speech-language pathologists (SLP) may help with dry throat, hoarseness and related vocal cord problems. These issues may particularly affect people who were on a ventilator.
Cognitive issues that develop can significantly impact a person’s ability to communicate. SLPs also address difficulties with writing, recalling words in conversation, communicating in a variety of settings and reduced organization of complex ideas and opinions.
The goal of therapy often includes returning patients to their previous levels of functioning. Therapy may also include teaching patients’ strategies to pace themselves and conserve energy as they continue to recover.
Who can Diagnose Patients for Long COVID?
There is no definitive test or process to determine if a person has long COVID. In many cases, screening includes a combination of medical history and symptom review. Primary care doctors and rehabilitative therapists may consider several factors, such as:
- History of COVID infection
- Symptoms present
- Exercise tolerance test
- Lying and standing blood pressure and heart rate
- Underlying medical conditions present
Continuing to have certain symptoms, such as fatigue, months after having COVID with no other known cause is a red flag.
Identification of patients with long COVID may come from both physicians and therapy staff.
“We may consider symptoms a person continues to have after recovering from COVID,” said Richardson. “If symptoms continue for three months post-infection, therapy is indicated.”
Who is at Risk for Long COVID?
According to research by the National Institute of Health, people with underlying health conditions, such as asthma, diabetes, autoimmune disorders or obesity, have an increased risk of developing long COVID.
Additional factors that increase risk include:
- Being unvaccinated
- Adults between 35-49
- Gender – women are at higher risk of contracting long COVID
Although researchers have identified certain risk factors, anyone with a COVID-19 infection can develop long COVID. This includes people with a mild infection.
“It does appear that having a lengthy ICU stay or being placed on a ventilator increases the likelihood of long COVID,” said Tim Dellwo, DPT, OCS, FAAOMPT, a board-certified orthopedic physical therapist at Brooks Rehabilitation. “But we also see people with long COVID who were not hospitalized during their COVID infection. These patients recovered at home and still have lingering COVID symptoms. So, the severity of the initial COVID infection is not the only thing that affects whether someone develops long COVID.”
There is still so much to learn about this condition. But becoming educated is an important step to recognize symptoms and understand how to get help.
How Rehabilitative Therapists Determine Treatment for Long COVID
Because information for long COVID continues to emerge, specific treatment protocols also continue to evolve. Therapists use their knowledge in similar areas to create a treatment plan.
They may draw from other treatment ideas to provide therapy for patients with long-COVID. For example, fatigue is also a common complaint of many other conditions. Therapists use similar methods of therapy to address fatigue in people with long COVID as they do with other causes of fatigue.
Pulling from evidence-based therapies to treat symptoms helps develop an effective treatment plan to in easing COVID symptoms.
“Patient situations differ,” said Dellwo. “But we use similar treatments for fatigue, balance and improved strength in people with long COVID as with other conditions. But because COVID is a respiratory illness, we need to closely monitor cardiac and respiratory response to exercise.”
Where Does Long COVID Treatment Take Place?
Similar to treating other types of injuries and condition, the treatment setting may vary.
“The severity of symptoms does not really determine treatment setting when dealing with long-COVID,” said Dellwo. “Exceptions exist, such as if someone is hospitalized for severe symptoms, including heart and lung problems. Insurance, specific treatment plan and personal preference may also affect treatment setting.”
Rehabilitative treatment settings may include:
Inpatient: Inpatient PT involves dedicated therapy sessions during a hospital stay. The frequency of therapy varies. The goals of inpatient physical therapy may differ from outpatient. Inpatient PT may focus on ensuring the patient is safe to go home or determine if they need to go to a rehab facility.
Outpatient clinic: Once patients do not require hospitalization, their doctor may recommend physical therapy in the outpatient clinic. Therapists may work with patients to return to normal activities and improve fatigue. One difference in the outpatient clinic, patients often feel better than they did during their hospital stay. This may result in more energy to perform therapy.
Home health: Home health involves therapy in a person’s home. This provides convenience and a greater sense of independence as a person recovers.
How Brooks Can Help
If you or a loved one is suffering from symptoms of long COVID, Brooks’ multi-disciplinary therapy team can help. Through our individualized approach for therapy treatment, we will work with you to develop a plan that will help you reach your recovery goals and empower you to your highest participation in life.
Request our services on our Become a Patient page.


