The Leader in Stroke Rehabilitation

Back to physical health resource hub
Someone has a stroke every 40 seconds in the United States, with some of the highest per capita stroke hospitalization rates occurring in the Southeast. Brooks Rehabilitation has received national recognition for our stroke rehabilitation program with our commitment to using the latest in clinical staff education and training, cutting-edge technology and ground-breaking research.
A Diversity of Programs and Resources
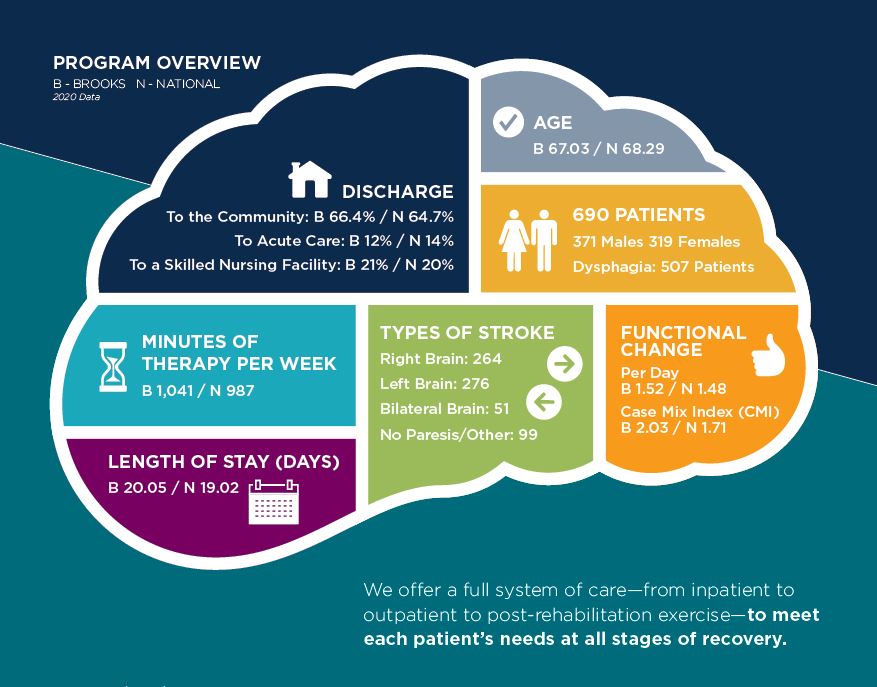
Every year, Brooks treats nearly 700 stroke survivors in our acute inpatient rehabilitation hospital alone – helping patients and their loved ones rebuild their lives and achieve their goals. This places Brooks as the number one stroke rehabilitation provider in Florida and the Southeastern U.S. and in the top ten in the country.
 Cassandra List, MD, joined Brooks two years ago and is Medical Director for the Stroke program and Spasticity program at Brooks Rehabilitation Hospital – University Campus. “When you come into a system like Brooks with a great reputation for providing exceptional patient-centered care, you are honored to be here. Then to see how many resources I can provide my patients with and actually see my patients improve because of those resources, has been even more rewarding. Just because they leave the hospital, their rehab doesn’t stop. It’s the diversity of the programs and resources available to our patients that really makes a difference.”
Cassandra List, MD, joined Brooks two years ago and is Medical Director for the Stroke program and Spasticity program at Brooks Rehabilitation Hospital – University Campus. “When you come into a system like Brooks with a great reputation for providing exceptional patient-centered care, you are honored to be here. Then to see how many resources I can provide my patients with and actually see my patients improve because of those resources, has been even more rewarding. Just because they leave the hospital, their rehab doesn’t stop. It’s the diversity of the programs and resources available to our patients that really makes a difference.”
Brooks offers a true stroke continuum of care: inpatient, outpatient, skilled nursing, home health and an array of community programs not found elsewhere. A person can enter the Brooks stroke continuum at any point and at any time, to get the rehabilitation help they need for the best possible outcome.
In many cases, Brooks will begin working with a patient well after their stroke occurred and after they may have received rehabilitation elsewhere. “I’ve seen stroke patients who had their stroke a year ago, five years ago, 10 years ago and for whatever reason they did not receive complete – or any – rehabilitation services,” said Dr. List. “Now they’ve been referred to Brooks. It’s bittersweet in the sense that I wish we could have offered services to them earlier, but it’s also exciting to know we still have so much we can offer them.
For example, maybe they get referred for their spasticity (muscle tightness in the arms or legs) after they’ve had the stroke. And yes, we certainly address ways to get them walking better or make it easier to get dressed. But we’ll go further and interview deeper. Maybe the patient feels their thinking isn’t quite right… well, let’s get a neuropsychological evaluation to understand their thought processing, memory and attention. Do they need additional physical or occupational therapies to address limitations? Maybe they’re still having trouble with their speech or language ability and they never had intense speech therapy, I can refer them to a specialist for that.
So, they might come into Brooks with one issue that they would like addressed, but, as a rehabilitation physician, my job is to look at the whole picture of their rehabilitation and work with the team to determine what we can do to help optimize their recovery, wherever they are in that process.”
Stroke Recovery Pathway: Ensuring the Same Quality of Care Throughout the System
It’s a priority at Brooks to ensure that this high quality and caliber of care exists throughout the entire Brooks system. That’s the impetus behind the “Recovery Pathway” program. Due to the large volume of stroke patients Brooks treats, stroke care is the initial diagnosis being addressed.
It’s important to note that a Recovery Pathway does not mean standardized or “cookie-cutter” care, even if of a high quality. “The plan of care for each stroke patient is individualized to that patient, because even a stroke in the same area of the brain can affect two people differently,” said Dr. List. “We have a customized plan of care that’s developed by our interdisciplinary team for that specific patient and the specific needs of that patient. But the Recovery Pathway is an effort, within that individual care, to make sure that each of the patients are receiving the same quality of care throughout the system. So, if you’re being treated for stroke in our rehabilitation hospital, when you transition home, we want the communication in place with our home health team to ensure you’re getting the same degree of expertise, focused specifically on your stroke, that you received as an inpatient.”
 Rhonda Flores, PT, Therapy Manager of Clinical Work at Brooks Rehabilitation Hospital – University Campus, is spearheading the Recovery Pathway program. “The Stroke Recovery Pathway came from the realization that we wanted our system to be unified in the way we approach the care of our stroke patients. Having the same high level of care, with the use of information, technology and the evidence-based research, is the Brooks culture we want to solidify.”
Rhonda Flores, PT, Therapy Manager of Clinical Work at Brooks Rehabilitation Hospital – University Campus, is spearheading the Recovery Pathway program. “The Stroke Recovery Pathway came from the realization that we wanted our system to be unified in the way we approach the care of our stroke patients. Having the same high level of care, with the use of information, technology and the evidence-based research, is the Brooks culture we want to solidify.”
Under Flores, there are two fundamental pillars for the Stroke Recovery Pathway:
- Brooks will apply neuroplasticity principles in every single patient’s treatment. Neuroplasticity is the ability of the brain to compensate and adjust to changes, like a stroke or injury, by forming new neural connections over time. The three principles of focus are intensity, salience and specificity.
- Brooks will use outcome measures to track the patient’s progress, so we can see the progress that they’ve made at any one point and throughout the system. Clinicians understand the importance and the need to do outcome measures, pre and post, using evaluations that are evidence-based for stroke patients.
In order to adapt this to each setting, we must define best practice as it relates to inpatient, home health, outpatient and aging services and develop strategies to incorporate those guiding principles into the care provided.
Investing in Education: The Clinical Practice Enhancement Program
The Pathway Program falls under the umbrella of the Clinical Practice Enhancement Program (CPE). This program is spearheaded by the Brooks Institute of Higher Learning (IHL), led by the CPE coordinator, Jackie Osborne, DPT, GCS.
The program is a system-wide professional development program for clinicians who work directly with patients. Brooks realized that the day-to-day operations of clinical practice can become so busy that it’s often challenging for clinicians to learn new ideas and implement new strategies. The CPE program is designed to help clinicians do just that, to stay cutting edge with the services they deliver by providing them with the resources needed to implement evidence-based best practices every day with every patient.
The first cohort group under CPE are clinicians who work with stroke patients – including 120 people in home health, 50 people at our rehabilitation hospital and 40 people who work with outpatients. They are all getting training specific to the management of stroke patients.
Sara Cristello PT, DPT, is the Director of Clinical Operations at Brooks. The IHL is leading the CPE program, in collaboration with Brooks subject matter experts and leaders from across the enterprise who are helping develop it. “There’s no organization in the U.S., perhaps the world, that we know of that’s doing this type of education for all clinicians across the entire system,” said Cristello. “It’s a robust program that includes face-to-face education, self-study courses and presentations, monthly group discussions and in-person mentoring. The program is during work hours. We’re carving out time for employees to invest in their clinical skillset to become experts in their fields for the betterment of our patients. It’s for all employees, not just those who choose to do a residency or fellowship. It’s a huge differentiator for Brooks.”
“This idea of clinical practice enhancement that is system-wide for the professional development of clinicians is a novel concept that has never been applied before in this way. At Brooks, we are leading the way with this innovative program and taking the concept of experiential learning in the clinical setting and creating a powerful way to integrate evidence with practice,” said Osborne.
As Important as the Physical: The Mental Health Side of Stroke
Mood is a large component of stroke recovery. The mental health of a stroke patient can be affected in two ways – having to adjust to how their body may have changed and how their life may have changed and/or the fact that the actual areas of emotion in the brain may have been affected by the stroke.
“Usually, it’s a bit of a combination of both,” said Dr. List. “So, there’s a lot of education we provide to patients to make sure they’re aware of what they may go through emotionally – that their emotions may be altered. It’s not something to ignore because mood plays a big role in functioning and therefore recovery.”
 Russell Addeo, PhD, is a neuropsychologist and Director of Behavioral Medicine at Brooks Rehabilitation. “The majority of people who have had a stroke will at some point develop depression. It could be related to the severity of the stroke, or it could be related to a prior history of depression.” If a stroke patient is tired, sad or not sleeping well, they’ll lose motivation. They won’t do as well at rehabilitation because they’re not going to want to participate. If depression isn’t treated, you could have worse outcomes not only in terms of rehabilitation, but also worse outcomes in terms of survival. The survival rate for people with untreated post-stroke depression is lower than those who’ve had the advantage of mental health resources.
Russell Addeo, PhD, is a neuropsychologist and Director of Behavioral Medicine at Brooks Rehabilitation. “The majority of people who have had a stroke will at some point develop depression. It could be related to the severity of the stroke, or it could be related to a prior history of depression.” If a stroke patient is tired, sad or not sleeping well, they’ll lose motivation. They won’t do as well at rehabilitation because they’re not going to want to participate. If depression isn’t treated, you could have worse outcomes not only in terms of rehabilitation, but also worse outcomes in terms of survival. The survival rate for people with untreated post-stroke depression is lower than those who’ve had the advantage of mental health resources.
The fact that Brooks provides comprehensive care from a psychological perspective, in addition to the physical recovery, differentiates us from other systems,” said Dr. Addeo. “We provide psychological services acutely at the Brooks hospital, where our psychologists and neuropsychologists assess and treat depression and any additional challenges the patient may have while they’re here.
At other points in the continuum, our Brooks physicians will refer patients to our psychological services. Our physicians may consider prescribing stroke patients an anti-depressant medication and then psychological services will help with managing and coping with the consequences of the stroke and dealing with any depression.”
“It’s all connected,” said Dr. List. “At Brooks, we know we can’t address just individual pieces of stroke recovery. They all work together. In rehabilitation, we work in an interdisciplinary team with physical, occupational, speech and cognitive therapists, as well as neuropsychologists. We each have our areas of expertise and we work together to get the best results – the best recovery or chance of recovery – for our stroke patients.”
Stroke Beyond Recovery
Brooks has the experience and experts to help stroke survivors recover. Brooks provides more specialized, focused stroke rehabilitation than others offering the most innovative, scientifically supported treatments available.
Patients are offered the newest, state-of-the-art equipment and innovative technology with proven outcomes for stroke survivors. As a research entity studying stroke recovery, Brooks helps determine the best treatment techniques.